Atrial Fibrillation and Stroke Prevention
What is Atrial Fibrillation?
Atrial fibrillation is a quivering or irregular heartbeat, or arrhythmia. Atrial fibrillation, also known as AFib or AF, can lead to blood clots, stroke, heart failure and other heart-related complications. Over 12 million people are projected to have AFib by 2030.
Here’s how patients have described their experience...
My heart flip-flops, skips beats, and feels like it’s banging against my chest wall, especially if I’m carrying stuff up my stairs or bending down.
I was nauseated, light-headed, and weak. I had a really fast heartbeat and felt like I was gasping for air.
I had no symptoms at all. I discovered my AFib at a regular check-up. I’m glad we found it early.
What happens during AFib?
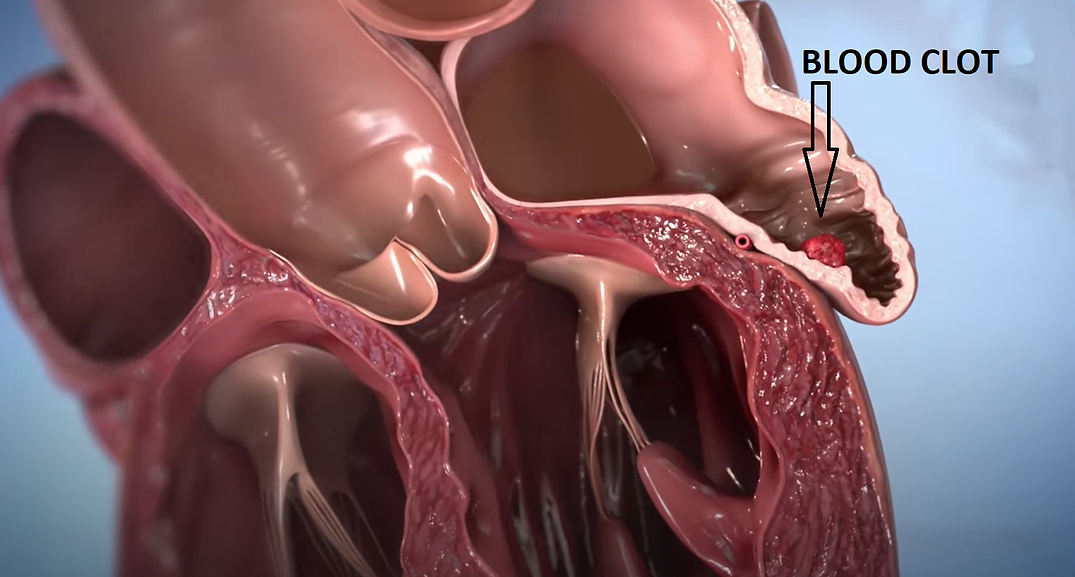
Normally, your heart contracts and relaxes to a regular beat. In AFib, the upper chambers of the heart, or the atria, beat irregularly. Since there is not enough blood being pumped out of the atria, blood pools in the area.
This pooled blood can clot – which can be extremely dangerous. (See Image)
If this blood clot forms, it can be pumped from the heart and to the brain. This blocks the blood supply to the brain and causes a stroke.
About 15% to 20% of people who have strokes have this heart arrhythmia. The clot risk is why patients with this condition are prescribed blood thinners*.
Untreated AFib doubles the risk of heart-related deaths and is associated with a fivefold increased risk for stroke. Yet many people are unaware that AFib is a serious condition.
AFib treatment saves lives and lowers risks
If you or someone you love has AFib, learn more about what it is; why treatment can save lives; and what you can do to reach your goals, lower your risks and live a healthy life.
If you think you may have AFib, here are your most important steps:
1. Know the symptoms
2. Get the right treatment
3. Reduce your risk for stroke and heart failure

Who is at Risk for Atrial Fibrillation?
People who have one or more of the following conditions are typically at higher risk for AFib:
• Advanced age: The number of adults developing AFib increases markedly with older age. AFib in children is rare, but it can happen.
• High blood pressure: Longstanding, uncontrolled high blood pressure can increase your risk for AFib.
• Underlying heart disease: This includes anyone with heart disease, including valve problems, hypertrophic cardiomyopathy, acute coronary syndrome, Wolff-Parkinson-White syndrome and a history of heart attack. Additionally, AFib is the most common complication after heart surgery.
• Drinking alcohol: Binge drinking (having five drinks in two hours for men, or four drinks for women) may put you at higher risk for AFib.
• Family history: Having a family member with AFib increases your chances of being diagnosed.
• Sleep apnea: Although sleep apnea isn’t proven to cause AFib, studies show a strong link between obstructive sleep apnea and AFib. Often, treating the apnea can improve AFib.
• Athletes: AFib is common in athletes and can be triggered by a rapid heart rate called a supraventricular tachycardia.
• Other chronic conditions: People with hyperthyroidism, diabetes, asthma and other chronic medical problems also are at risk.
What are the Symptoms of Atrial Fibrillation?
Sometimes people with AFib have no symptoms and their condition is only detectable upon physical examination. Others may experience one or more of these symptoms:
• General fatigue
• A rapid and irregular heartbeat
• Fluttering or “thumping” in the chest
• Dizziness
• Shortness of breath and anxiety
• Weakness
• Faintness or confusion
• Fatigue when exercising
• Sweating
• Chest pain or pressure
Are there different types of AFib?
Yes, there are different types of AFib!
The symptoms are generally the same, although the duration of the AFib and underlying reasons for it can help medical practitioners classify the type of AFib problems.
• Paroxysmal fibrillation is when the heart returns to a normal rhythm on its own, or with intervention, within seven days of abnormality. People who have this type of AFib may have episodes only a few times a year or their symptoms may occur every day. These symptoms are very unpredictable and can often turn into a permanent form of AFib.
• Persistent AFib is an irregular rhythm that lasts for longer than seven days. This type of AFib will not return to a normal sinus rhythm on its own and will require some form of treatment.
• Longstanding AFib is when the heart is consistently in an irregular rhythm for longer than 12 months.
• Permanent AFib occurs when the condition lasts indefinitely, and the patient and doctor have decided not to continue trying to restore a normal rhythm.
• Nonvalvular AFib is AFib not caused by a heart valve issue.
Over a period of time, paroxysmal fibrillation may become more frequent and longer lasting. This sometimes leads to permanent or chronic AFib.
Treatment and Prevention of Atrial Fibrillation
Medications for atrial fibrillation
Doctors often prescribe medications to prevent and treat blood clots that can lead to a stroke. They may also prescribe additional drugs to control your heart rate and rhythm, and recommend medications in conjunction with other treatments.
The heart rhythm can be more difficult to control. The longer you have untreated atrial fibrillation (also called AFib or AF), the more difficult it is to reestablish a normal rhythm.
Medication options may include *blood thinners, heart rate controllers, and heart rhythm controllers. The lists here are not intended to be comprehensive, and we encourage you to revisit this page often to keep up with the newest in AFib medication options.
Your doctor will use an assessment scale called the CHA2DS2–VASc risk to determine whether you will need medication. The components of the scale are:
• Congestive heart failure
• Hypertension (the medical term for high blood pressure)
• Age (75 or older)
• Diabetes
• Stroke (prior episode)
• Vascular disease (prior heart attack, peripheral artery disease or aortic plaque)
• Age 65-74
• Sex (female)
Preventing Clots with medication (antiplatelets and anticoagulants)
Doctors prescribe drugs such as blood thinners to prevent blood clot formation or treat an existing blood clot.
Examples include:
• Warfarin
• Other Food and Drug Administration-approved anticoagulants such as dabigatran, rivaroxaban, edoxaban, and apixaban (direct-acting oral anticoagulants)
• Aspirin (in rarer cases)
